Abstract
Background: Acute graft-versus-host disease (GVHD) remains a major obstacle for successful allogeneic stem cell transplantation (HSCT) from unrelated donors. Novel preventive regimens are thus needed. The proteasom inhibitor bortesomib has immune modulatory effects that were shown to be beneficial in several studies adding a short treatment course to the standard calcineurin/ methotrexate regimen in matched and mismatched unrelated donor transplant. Carfilzomib is a second generation irreversible proteasome inhibitor. It is more selective than bortesomib and was shown to be more effective in relapsed refractory multiple myeloma. However, there is no data on the effect of carfilzomib in GVHD prevention. We explored a novel regimen consisting of 2 doses of carfilzomib at 20 mg/m2, given on days 1 and 2 after HSCT combined with standard anti GVHD prophylaxis regimen of cyclosporine/ methotrexate. The study enrolled patients with acute myeloid leukemia (AML) in remission (CR) or patients with myelodysolastic syndrome (MDS) with less than 10% blasts, given a 10/10 or 9/10 matched unrelated donor transplant with fludarabine-based reduced-intensity or reduced-toxicity conditioning.
Patients and Methods: 20 patients, 8 male, 12 female, median age 63 years (range, 30-72) were recruited to the study. Fifteen patients had AML and 5 had MDS. Ten patients were in CR1, 5 in CR2 and 5 were previously untreated at the time of transplantation. The conditioning regimen included fludarabine combined with intravenous busulfan at reduced doses (n=6) or myeloablative doses (n=11) or with treosulfan (n=3). All patients were also given antithymocyte globulin (ATLG ,Grafalon ,Neovii, total dose 15 mg/kg). The donors were all unrelated donors and were 10/10 HLA matched (n=10) or 9/10 matched (n=5). Transplantation outcomes were compared to a historical group of 100 patients with similar patient and transplant characteristics given unrelated donor transplant with a standard anti GVHD cyclosporine/ methotrexate GVHD prevention regimen.
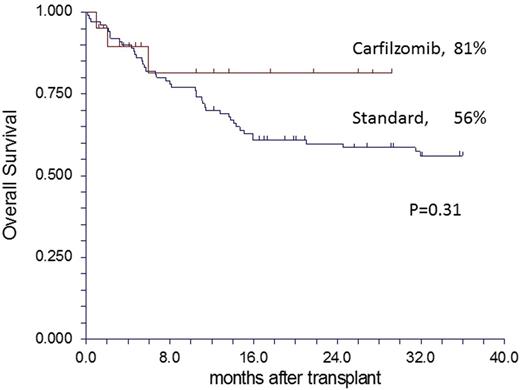
Results: Eighteen patients completed the planned two days of carfilzomib on day 1 and 2 post-transplant. One patient had only one dose and one none of the doses due to adverse events that dictated stopping treatment by protocol. The median follow-up is 11 months (range 1-29). All patients engrafted with a median of 15 days (range, 10-31) compared with 14 days (range, 9-23) in the control group (P=0.14). Mucositis grade ≥3 occurred in 60% and 24% of the study patients and historical controls, respectively (P=0.001). There was no difference in the rate of all other grade ≥3 organ toxicities, 20% and 30%, respectively (P=0.36). Acute GVHD grade II-IV occurred in only one patient in the study group, a cumulative incidence of 5% (95%CI, 1-34) compared with 39% (95%CI, 30-50) in the control group (P=0.007). Chronic GVHD occurred in 5 patients in the study group , a cumulative incidence of 58% (95%CI, 30-100) compared with an incidence of 41% in the historical controls (95%CI, 33-52) (P=0.58). Notably, all study pts had mild chronic GVHD while, the incidence of moderate to severe chronic GVHD was 0% and 18% (95%CI, 11-30), respectively (P=0.17). Non-relapse mortality (NRM) occurred in 2 patients on study, one died of acute GVHD and the other of multi-organ failure. The cumulative incidence of NRM was 11% (95%CI, 3-39) and 22% (95%CI, 15-32), in the study and control group, respectively (P=0.68). Finally, only one study patient relapsed, cumulative incidence 8% (95%CI, 1-53), compared to 26% (95%CI, 18-36) in the historical controls (P=0.310). In all, 17/20 study patients are alive with an estimated 2-year survival of 81% (95%CI, 68-100) compared to 56% (95%CI, 46-66) in the control group, respectively (Figure, P=0.31).
Conclusions: Carfilzomib in addition to standard cyclosporine/ methotrexate as anti GVHD prophylaxis after unrelated- donor transplant is safe and allows better prevention of acute GVHD without compromising the graft-versus-leukemia effect. The add on of carfilzomib results in favorable outcome. Larger studies with longer follow-up are required to confirm these initial promising results.
No relevant conflicts of interest to declare.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal